An Experimental Pharmaceutical Treatment for Long Covid (Part 2: Molecular-Level Impacts)
Part 2: Molecular-Level Impacts
A new Experimental Pharmaceutical Treatment for Long Covid, called Triple Anti-Coagulant Therapy, has been tested in a small study of Long Covid Patients (see Ref below).
Last week in Part 1, I talked about the Impact on Symptoms of Triple Anti-Coagulant Therapy.
Now this week, I want to talk about the:
Molecular mechanisms of action of the drugs that make up the Triple Anti-Coagulant Therapy,
Effect of the treatment at the molecular level on microclotting and platelet hyperactivation, and
Side effects that were observed during the study.
As a reminder (and disclaimer), this information has only been reported in a preprint (Link below in the References). It has NOT undergone peer-review and has NOT been formally published in a journal.
Now, without any further delay…
Triple Anti-Coagulant Therapy: Component Drugs & Mechanisms of Action
What is Triple Anti-Coagulant Therapy?
Triple Anti-Coagulant Therapy is made of three main components - one anti-coagulant drug (apixaban) and two different platelet activation inhibitors (aspirin and clopidogrel), each of which has a different mechanism of action. The drugs, their doses & schedule, and mechanisms of action are in the table below.
Let’s look at the mechanisms of action:
Apixaban, the anti-coagulant, is an inhibitor of Factor Xa (pronounced “10-A”), which is a key enzyme in the Coagulation Cascade that forms clots. Factor Xa is the enzyme that modifies fibrinogen to make fibrin, which then polymerizes into clots (see here for a review on clotting mechanisms). So inhibiting Factor Xa decreases the ability for clots to form naturally. And remember, while the Covid Spike Protein can create microclots without needing Factor Xa, when that enzyme is present the microclots get much worse (see here). So inhibiting the endogenous clot formation process (by inhibiting Factor Xa) should reduce the overall creation of microclots in the Long Covid patients.
Aspirin, as we have previously discussed, inhibits platelet activation by inhibiting the COX-1 and COX-2 enzymes. This inhibition of COX-1/2 by aspirin directly blocks the production/release of thromboxane A2 and prevents activation of the TP receptor on the platelet cell membrane. Decreasing platelet hyperactivation prevents the activated platelets from sticking to the microclots, reducing the size of the microclots and allowing them to be broken down more easily by the natural process of fibrinolysis.
Clopidogrel also inhibits platelet activation, but does so by inhibiting the P2Y1 and P2Y12 receptors on the platelet cell membrane. Clopidogrel binds directly to the P2Y1/12 receptors and blocks the binding of the natural activating ligand for these receptors (ADP), thereby trapping the receptors in the inactive, unactivated state. This inhibition of platelet hyperactivation by clopidogrel works synergistically with the inhibition of platelet hyperactivation by aspirin, significantly reducing the contribution of platelet hyperactivation to microclotting and the Long Covid phenotype.
You’ll also notice that there is a forth drug, pantoprazole, listed as part of the “Triple” Anti-Coagulant Therapy. The pantoprazole doesn’t have any effect on microclots or platelet hyperactivation. It’s there as gastric protection to address the GI irritation and discomfort that is a side effect of the aspirin. We’ll talk about this more below in the Side Effects section below.
Experimental Pharmaceutical Treatment for Long Covid
From Part 1, remember that Pretorius, Kell, and coworkers examined a cohort of 91 Long Covid patients that they treated with Triple Anti-Coagulant Therapy.
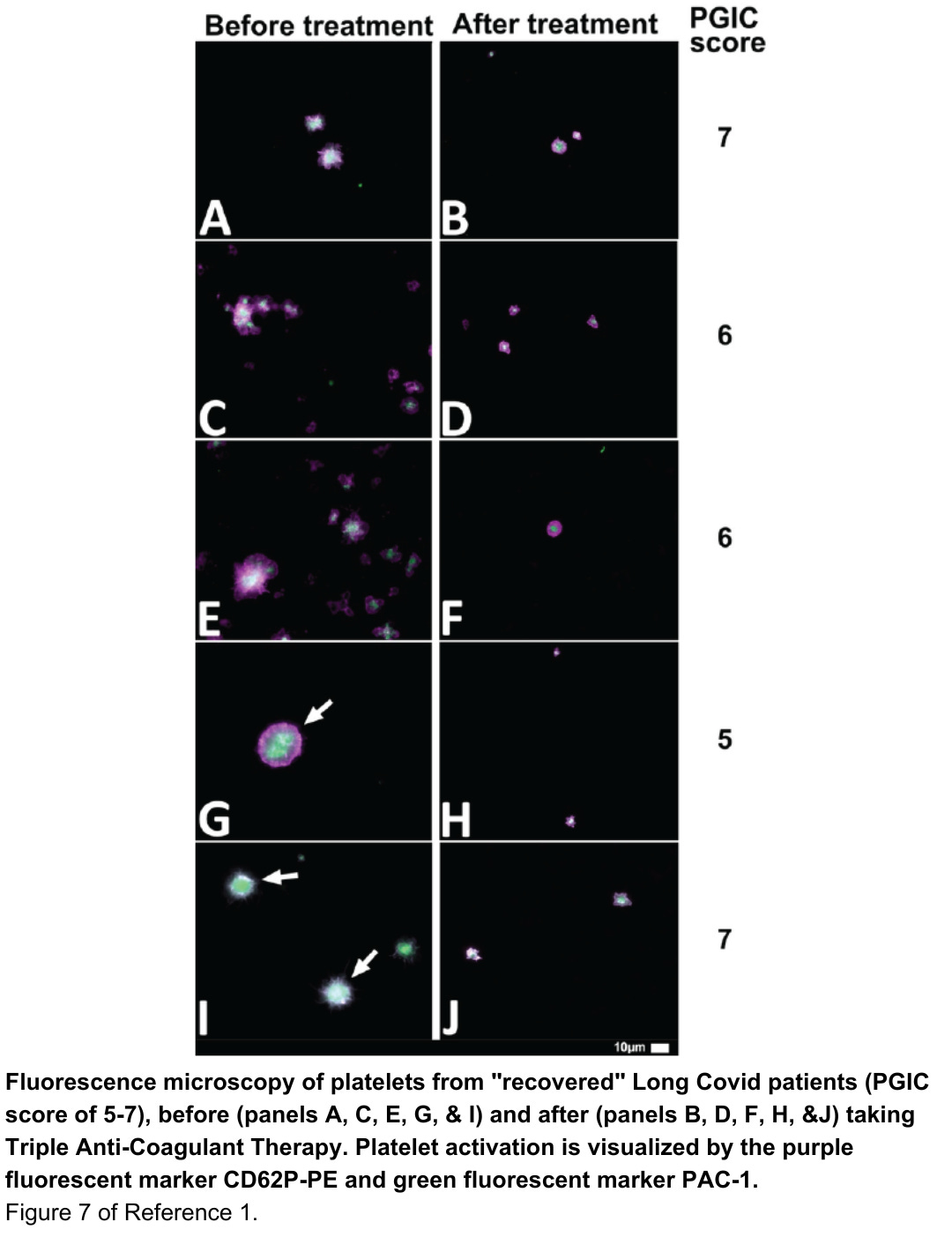
Blood samples were taken from the patients before and after treatment. Blood samples were evaluated by fluorescence microscopy for microclots (thioflavin T (ThT), see more info here and here) and platelet hyperactivation (CD62P & PAC-1 fluorescent markers, see more info here).
Prior to starting treatment, all 91 patients were confirmed to have microclots and platelet hyperactivation, the molecular hallmarks of Long Covid.
Remember also the Findings from Part 1:
Finding #1: For each Long Covid symptom evaluated, >74% of patients saw that symptom resolve and no longer be present.
Finding #2: 80% of the Long Covid patients (73 of 91 patients) showed enough of an improvement in their Patient Global Impression of Change (PGIC) Scale to be considered “recovered” from Long Covid.
Results from the Study (continued from Part 1)
Finding #3: Triple Anticoagulant Therapy reduced microclotting and platelet hyperactivation in the 80% of Long Covid patients judged to be “recovered” based on their PGIC Score. [PGIC scores of 5-7 were considered “recovered”]
The images below used fluorescence microscopy and the appropriate stain to detect microclotting and platelet hyperactivation. In each figure, the left-hand column of images shows patient samples before treatment and the right-hand column of images shows patient samples after treatment in patients whose symptoms improved.
These “before” and “after” treatment samples are all from patients that were judged to be “recovered” from Long Covid, based on their PGIC score having improved to the 5-7 range and their symptoms having resolved (note the PGIC scores along the right side in the figures).
This data shows that the molecular level markers for Long Covid (microclotting and platelet hyperactivation) also resolved along with the Long Covid symptoms.
That’s a clear win for Triple Anti-Coagulant Therapy.
What about the patients that didn’t recover on Triple Anti-Coagulant Therapy?
Finding #4: Triple Anticoagulant Therapy DID NOT reduce microclotting and platelet hyperactivation in the 20% of Long Covid patients that were judged to have “NOT recovered” based on their PGIC Score [scores of 1-4]
Fluorescence microscopy and the appropriate stain were again used to detect microclotting and platelet hyperactivation in blood samples from the “NOT recovered” patients. Again in this figure, the left-hand column of images shows patient samples before treatment and the right-hand column of images shows patient samples after treatment in patients whose symptoms improved. Platelet hyperactivation is examined in panels A-D and microclotting in panels E-H. Notice the PGIC score of 2 for all these “NOT recovered” patients.
This data shows that in the “NOT recovered” patients with a low PGIC score, both the microclots and the platelet hyperactivation persist, despite having been on the Triple Anti-Coagulant Therapy treatment. Unfortunately for these patients, the molecular-level effects and the symptoms both continue after treatment.
More studies will likely have to be done to figure out why Triple Anti-Coagulant Therapy didn’t work for these patients and if an alternative treatment may help them.
Side Effects
Based on the mechanisms of action of the drugs in the Triple Anti-Coagulant Therapy, there are two major side effects to be concerned with:
Problems with bleeding, bruising, and other issues related to coagulation
Gastric irritation and bleeding from the aspirin
Let’s look at these and whether they were an issue in this 91-patient study.
Coagulation Side Effects
Whenever people are taking anti-coagulants and platelet activation inhibitors, there is always a concern that blood clotting will be impaired if they are injured - by cutting themselves for example. Or from a nosebleed. This would lead to excessive bleeding, because clots won’t form to stop the bleeding at the sight of injury.
A second side effect of anti-coagulants and platelet activation inhibitors is that people bruise more easily. Even slight bumps or a stumble may cause discolorations of the skin from bleeding that may occur underneath.
In the Triple Anti-Coagulant Therapy study, the following coagulation side effects were observed:
75 patients (82%) experienced bruising (but no need for medical attention)
5 patients (5.5%) experienced nosebleeds
3 patients (3.3%) reported excessive bleeding after a cut (1 patient required medical attention)
2 female patients (3.7%) reported increased menstrual bleeding
Gastric irritation and bleeding
Inhibition of the COX-1/2 enzymes by aspirin has long been known to cause side effects in the GI tract, including not only discomfort but also bleeding that can lead to serious illness and require medical attention. Pantoprazole, a proton pump inhibitor that helps decrease these effects, was administered as part of the Triple Anti-Coagulant Therapy to address this common side effect of aspirin.
So was gastric irritation and bleeding a side effect seen in the 91 Long Covid patients in the study? Just 1 patient was reported to have a GI issue. A “NOT recovered” patient with a PGIC score of 1 had a GI bleed and required a blood transfusion. No other GI side effects were reported in the preprint.
This summarizes the molecular effects of Triple Anti-Coagulant Therapy in this study of 91 Long Covid patients from Pretorius, Kell, and coworkers. Remember this is a preprint - see the Disclaimer above and the Reference below.
To me, there seem some obvious next questions:
What’s the next step in evaluating Triple Anti-Coagulant Therapy in Long Covid?
Can patients get access to Triple Anti-Coagulant Therapy?
I’ll be talking about the answers to those questions in my next post. Stay tuned!
Leave me a comment below and let me know what you think of this post.
To follow my research, subscribe to my Substack!
And if you like watching videos, check out and follow my TikTok!
Reference
Treatment of Long COVID symptoms with triple anticoagulant therapy. Research Square Pre-Print 2023, rs-2697680/v1. https://doi.org/10.21203/rs.3.rs-2697680/v1